Schizoaffective Disorder Treatment in Pennsylvania
What is Schizoaffective Disorder?
Schizoaffective disorder is a chronic mental health condition characterized by a combination of symptoms of both schizophrenia and mood disorders, such as major depressive disorder or bipolar disorder. This condition is relatively rare, affecting less than 1% of the general population, and tends to emerge in early adulthood.
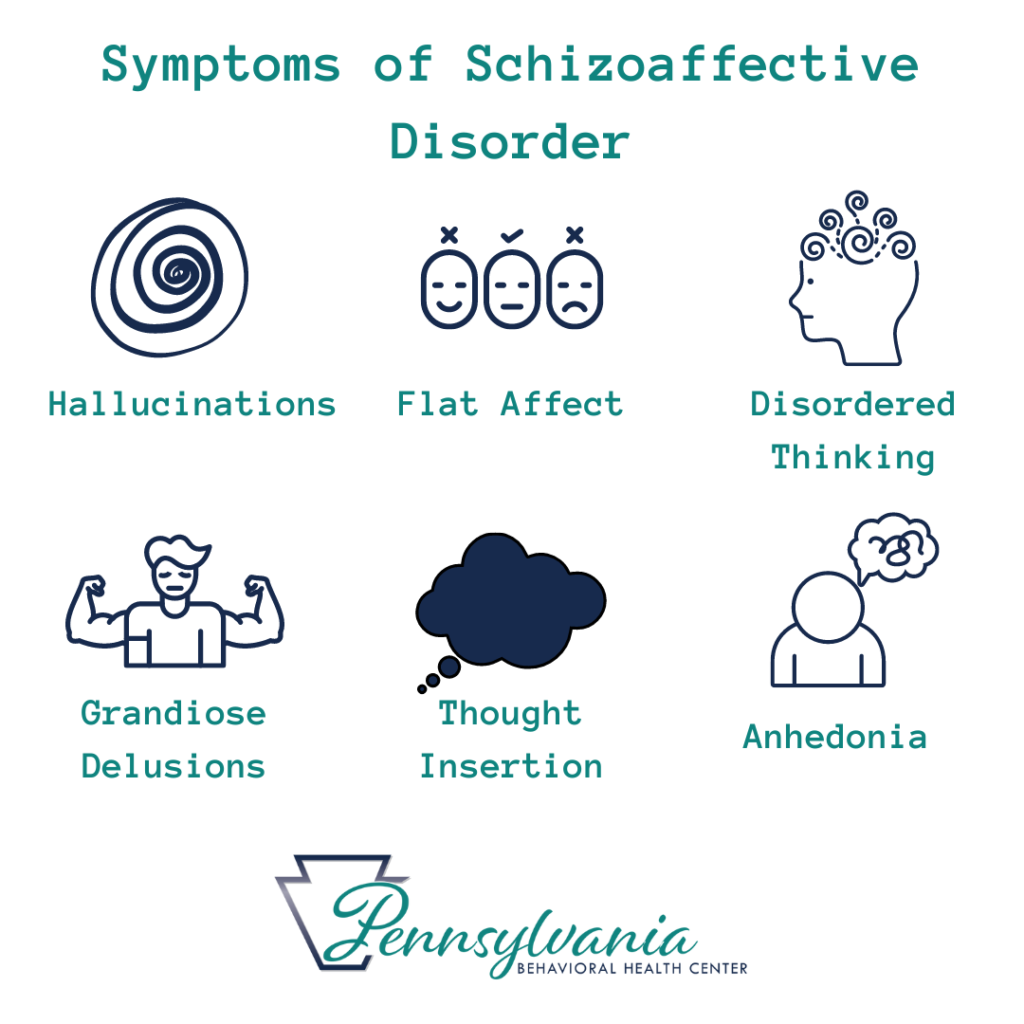
The symptoms of schizoaffective disorder can vary widely, but typically include hallucinations, delusions, disorganized thinking, and mood disturbances such as depression or mania. The symptoms must be present for a significant period of time, typically at least six months, in order for a diagnosis of schizoaffective disorder to be made.
There is limited information available on the prevalence of schizoaffective disorder, but research suggests that it may be more common in women than men. One study found that women with schizoaffective disorder were more likely to experience depressive symptoms, while men with the condition were more likely to experience manic symptoms (Source: National Institute of Mental Health).
How Does a Psychiatrist Diagnose Schizoaffective Disorder?
The process of diagnosing schizoaffective disorder in Pennsylvania typically involves a thorough evaluation by a psychiatrist or other mental health professional. The diagnostic process may include the following steps:
Initial assessment: The psychiatrist will begin by conducting a thorough assessment of the individual’s symptoms and medical history. They will ask questions about the individual’s symptoms, such as when they started, how long they have been present, and how severe they are. They will also ask about any past or current medical conditions, medications, and substance use.
Diagnostic criteria: The psychiatrist will then use the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to determine if the individual meets the diagnostic criteria for schizoaffective disorder. To be diagnosed with schizoaffective disorder, an individual must have symptoms of both schizophrenia and a mood disorder (either depressive or manic) for a significant period of time, typically at least six months.
Physical exam: The psychiatrist may also conduct a physical exam to rule out any underlying medical conditions that may be contributing to the individual’s symptoms. They may also order laboratory tests, such as blood work or imaging studies, to further evaluate the individual’s physical health.
Psychological testing: The psychiatrist may also administer psychological tests to assess the individual’s cognitive and emotional functioning. These tests may include measures of memory, attention, and executive functioning, as well as assessments of mood and anxiety.
Collaborative approach: In Pennsylvania, the diagnostic process is often collaborative, involving input from other healthcare providers, such as primary care physicians or psychologists. This helps to ensure a comprehensive evaluation and accurate diagnosis.
Once a diagnosis of schizoaffective disorder has been made, the psychiatrist will work with the individual to develop a treatment plan tailored to their specific needs. This may involve a combination of medication, therapy, and support from loved ones. Regular follow-up appointments will also be scheduled to monitor the individual’s progress and adjust the treatment plan as needed.
What is the prognosis of someone with Schizoaffective Disorder?
The prognosis for individuals with schizoaffective disorder can vary widely, but in general, the condition tends to be chronic and can be difficult to treat. Medication, therapy, and support from loved ones are often necessary to help manage the symptoms and improve quality of life.
According to the National Alliance on Mental Illness, individuals with schizoaffective disorder are at a higher risk of suicide than the general population. In fact, research has found that up to 50% of individuals with schizoaffective disorder attempt suicide at some point in their lives, and up to 20% die by suicide (Source: American Journal of Psychiatry).
What is the cause of Schizoaffective Disorder?
The exact cause of schizoaffective disorder is not fully understood, but it is likely the result of a combination of genetic, environmental, and neurobiological factors. Some potential causes and risk factors that have been identified include:
Genetics: Schizoaffective disorder appears to run in families, and research has identified several genetic variants that may increase the risk of developing the condition (Source: Nature).
Neurobiology: Schizoaffective disorder is thought to involve abnormal functioning in several areas of the brain, including the prefrontal cortex, hippocampus, and amygdala. Neuroimaging studies have shown differences in brain structure and activity in individuals with the condition (Source: Current Psychiatry Reports).
Environmental factors: Exposure to certain environmental factors, such as viral infections or prenatal complications, may increase the risk of developing schizoaffective disorder (Source: Psychiatry and Clinical Neurosciences).
Substance use: Substance abuse, particularly of drugs like marijuana or amphetamines, may increase the risk of developing psychotic symptoms that can lead to a diagnosis of schizoaffective disorder (Source: Harvard Health Publishing).
Stressful life events: Traumatic or stressful life events, such as abuse or neglect, may also increase the risk of developing the condition (Source: Psychiatry and Clinical Neurosciences).
It is important to note that while these factors may increase the risk of developing schizoaffective disorder, not everyone who experiences them will go on to develop the condition. More research is needed to fully understand the complex interactions between these factors and how they contribute to the development of the disorder.
What kind of treatments are there for Schizoaffective Disorder?
Schizoaffective disorder can be a challenging condition to treat, and treatment typically involves a combination of medication and therapy. In Pennsylvania, there are several therapeutic modalities that have been shown to be effective in the treatment of schizoaffective disorder. These include:
Cognitive Behavioral Therapy (CBT): CBT is a type of therapy that helps individuals identify and change negative thought patterns and behaviors that may be contributing to their symptoms. In the case of schizoaffective disorder, CBT may focus on reducing symptoms of depression or anxiety, managing stress, and improving social skills.
Family Therapy: Family therapy involves working with the individual and their family members to improve communication, reduce stress, and promote healthy coping strategies. Family therapy can be particularly helpful for individuals with schizoaffective disorder, as family members can provide valuable support and help monitor the individual’s symptoms and treatment.
Group Therapy: Group therapy involves meeting with a group of individuals who are experiencing similar challenges. Group therapy can be a helpful way to build social skills, reduce isolation, and learn coping strategies from others who are going through similar experiences.
Psychodynamic Therapy: Psychodynamic therapy focuses on exploring the unconscious thoughts and emotions that may be contributing to the individual’s symptoms. Psychodynamic therapy can be a helpful way to understand the root causes of the individual’s symptoms and develop strategies for managing them.
Acceptance and Commitment Therapy (ACT): ACT is a type of therapy that helps individuals learn to accept difficult thoughts and emotions, rather than trying to avoid or suppress them. ACT can be a helpful way to build resilience and improve quality of life for individuals with schizoaffective disorder.
It is important to note that the most effective therapeutic modalities for schizoaffective disorder may vary from individual to individual, and a comprehensive treatment plan should be tailored to the individual’s specific needs and preferences. It is recommended to consult with a mental health professional to determine the most effective treatment plan for each individual.
What Medications are Effective Against Schizoaffective Disorder?
Schizoaffective disorder is a complex mental health condition that typically requires a combination of medication and therapy for effective treatment. In Pennsylvania, there are several types of medications that have been shown to be effective in treating the symptoms of schizoaffective disorder. These include:
Antipsychotics: Antipsychotic medications are often the first-line treatment for individuals with schizoaffective disorder. These medications work by blocking dopamine receptors in the brain, which can reduce symptoms of psychosis such as delusions and hallucinations. Examples of antipsychotic medications include risperidone, olanzapine, and aripiprazole.
Mood Stabilizers: Mood stabilizers are medications that are typically used to treat bipolar disorder, but they can also be helpful in treating the mood symptoms of schizoaffective disorder. Mood stabilizers work by regulating the levels of neurotransmitters in the brain, such as serotonin and norepinephrine. Examples of mood stabilizers include lithium, valproic acid, and lamotrigine.
Antidepressants: Antidepressant medications can be helpful in treating the depressive symptoms of schizoaffective disorder. These medications work by increasing the levels of neurotransmitters in the brain, such as serotonin and norepinephrine. Examples of antidepressant medications include fluoxetine, sertraline, and bupropion.
Anxiolytics: Anxiolytics, or anti-anxiety medications, can be helpful in treating the anxiety symptoms of schizoaffective disorder. These medications work by increasing the activity of the neurotransmitter GABA in the brain, which can reduce anxiety and promote relaxation. Examples of anxiolytic medications include lorazepam, clonazepam, and alprazolam.
It is important to note that all medications come with potential side effects and risks, and the most effective medication for an individual may vary based on their specific symptoms and medical history. It is recommended to work closely with a mental health professional to determine the best medication regimen for each individual and to closely monitor the individual’s symptoms and medication response over time.
What is the Difference Between Schizoaffective Disorder, Schizophrenia, & Bipolar?
Schizoaffective disorder, schizophrenia, and bipolar disorder are all mental health conditions that can cause significant impairment in an individual’s daily life. However, they have distinct differences in terms of their symptoms and diagnostic criteria.
Schizophrenia is a chronic mental illness that typically manifests in early adulthood and is characterized by a range of symptoms, including hallucinations, delusions, disorganized thinking and speech, and social withdrawal. Schizophrenia is primarily a psychotic disorder, meaning that it is primarily characterized by symptoms of psychosis.
Bipolar disorder, on the other hand, is a mood disorder that is characterized by episodes of mania and depression. Individuals with bipolar disorder experience periods of elevated, manic or hypomanic mood, which can be accompanied by symptoms such as grandiosity, increased energy, and decreased need for sleep. They also experience periods of depression, which can be accompanied by symptoms such as feelings of sadness, hopelessness, and worthlessness.
Schizoaffective disorder is a hybrid of both schizophrenia and bipolar disorder. It is a chronic mental illness that is characterized by symptoms of both schizophrenia and mood disorders. Specifically, individuals with schizoaffective disorder experience episodes of both psychosis (such as hallucinations or delusions) and mood episodes (such as depression or mania). Unlike bipolar disorder, these mood episodes occur concurrently with symptoms of psychosis and are not independent of them.
In summary, while all three disorders can cause significant impairment in an individual’s daily life, schizophrenia is primarily a psychotic disorder, bipolar disorder is primarily a mood disorder, and schizoaffective disorder is a hybrid of both.
Sources:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
- National Institute of Mental Health. (2021, February). Schizophrenia. https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml
- National Institute of Mental Health. (2019, October). Bipolar disorder. https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
- National Institute of Mental Health. (2020, January). Schizoaffective disorder. https://www.nimh.nih.gov/health/topics/schizoaffective-disorder/index.shtml
- Rummel-Kluge, C., Kissling, W., & Leucht, S. (2008). Antidepressants for the treatment of schizophrenia? A systematic review and meta-analysis. Schizophrenia Research, 106(1), 1–15. https://doi.org/10.1016/j.schres.2008.07.023

